Lesson 6: Clinical Data collection and visualization challenges
Two key challenges in HIT:
- Data collection: efficiently and accurately collect high quality, comprehensive clinical data from busy and often computer-averse providers
- visualizing EHR data: in a way that supports the provider’s mental model
Ⅰ. Data Collection
Conflicts

- physicians are in the Data Business.
- medical records and record keeping receive minimal attention in medical training.
How Physicians collecting and using data:



- Subjective interviewing -> preliminary diagnosis
- Objective laboratory, imaging, and other tests.
- Based on subjective and objective data, assign the patient with one or more diagnoses;
- Develop a plan for managing them (e.g. prescribing medications, referral to specialists).
- Follow up and make adjustments.
- Coordination with other providers.
Three common sources of error:

- An Incomplete Knowledge Base - the physician can’t know everything
- An Error in Perception or Judgment - physicians are subject to human error, and
- A Lapse in Attention - Busy physicians are may not focus sufficiently on each case.
Mishandling of data might cost life and money
Electronic records themselves can be a new source of errors.
reason:

- Data standards are large and complex.
- An electronic version of the paper check off forms - long list which bounds to errors
Sources of electronic records error



- “active error” — the entry of inaccurate information.
- incorrect system defaults.
- a) provider may overlook the default value while charting.
- b) EHR “remembers” the values from a patient’s prior visit.
- fitting as much as possible onto each data entry screen.
- inconsistent data across locations. (different terms for the same thing or non-standard abbreviations or acronyms).
- Physicians may not record all the needed data
- hard to know which observations/events is definitive or even the most up-to-date.
M*Modal

- advanced medically specific voice recognition technologies.
- translate voice to text
- recognize clinical concepts in that text and codes them (using ICD9 and SNOMED-CT).
- M*Modal is a tool, it isn’t an EMR.
- The first EMR implemented M*Modal was PrimeSuite from Greenway Medical Technologies.


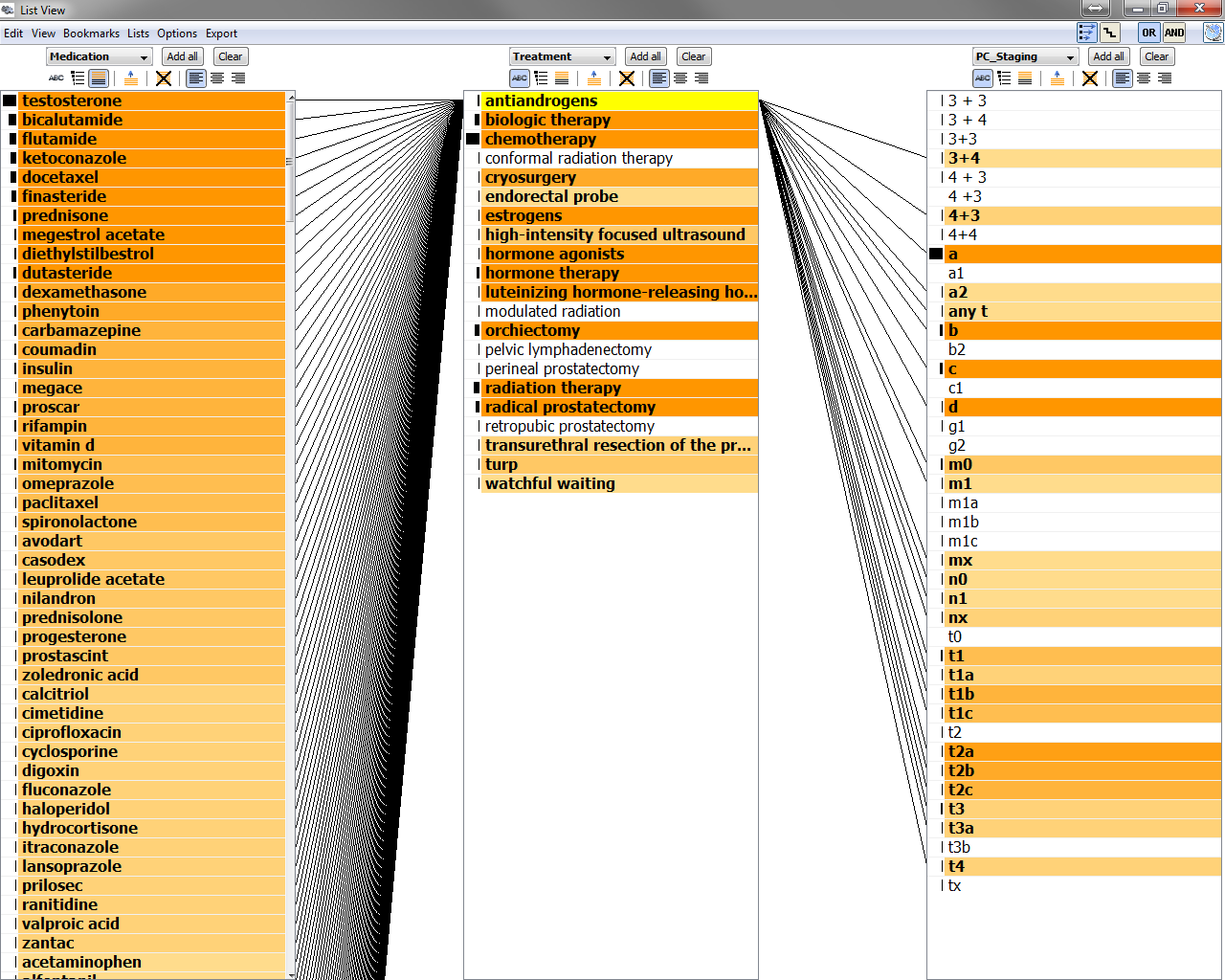
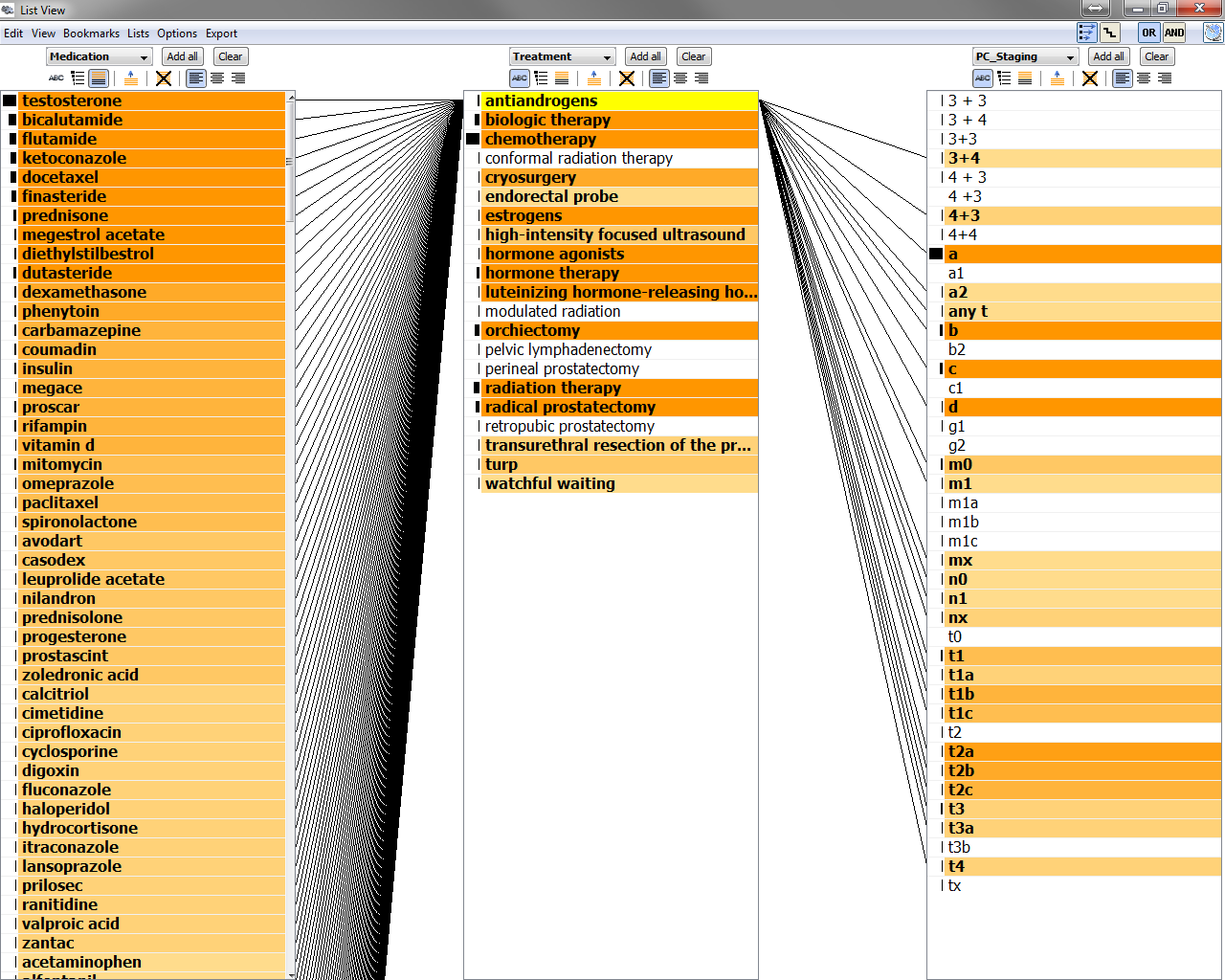
The SNOMED-CT browser.
Interview with M*Modal's chief scientist, Dr. Juergen Fritsch

Q1. Why M*Modal was not directly built in an EMR and how do you train the system?
A: It is intentional. We started with finding the technology with dictation and transcription in the backend and provide a drafted report for physicians to review and confirm, and use the drafted and the corrected report to train the system. After years of training, the system becomes useful for immediate audio recognition.
Q2. How hard it is to automatically find clinical concepts in verbal transcriptions and coded them into SNOMED?
A: dealing with the complex SNOMED ontology and challenges in natural language processing. Also, ambiguity of words with different meanings in different contexts is another thing to deal with.
Q3. How accurate is the system now?
A: Depends on usecase. It can be very accurate for some subset of SNOMED (e.g. for particular type of diseases). The accuracy rate is low if you try to encode the whole SNOMED-CT due to the complexity of it.
Q4. What technologies does M*Modal is using?
A: 1). Speech recognition: well-know machine learning models ( neural network, regression models, etc……). But we combine speech recognition technologies with natural language processing technologies. 2) coding to SNOMED: a lot of classifiers
Q5. How is it going with implementing M*Modal into the EMR system PrimeSuite from Greenway?
A: Physicians like storytelling style of data entry, so M*Modal is a great to extract information from verbal notes into structured information. More and more EMR vendors starts to invest in ways to preserve narrative type of data.
Q6. what 's the potential role of voice recognition technology in healthcare?
A: Physicians tends to create storylines and narratives around their patients. voice recognition technology is a way to help physicians enter this type of data into EMR systems.
Voice recognition technology can help to improve evidence based healthcare by identifying trends, facts in documents created by physicians. The information can be used to derive better treatment and accurate diagnosis for other patients.
The original M*Modal was founded by three Carnegie Mellon PhD's. It was acquired in 2011 by MedQuist, a much larger company, and the merged entity was renamed M*Modal. It filed for bankruptcy in 2014 but, so far as I can tell, its business was actually profitable but insufficient to pay the huge debt incurred as part of the merger so the purpose of the filing was to restructure the debt.
Machine learning in EMR technology

- Praxis by Infor*Med Corporation.
- Praxis learns how physician usually treats each problem and presents a note based on the most similar past patient(s).
- Each phrase is what Praxis calls a “clinical concept” : text descriptions as defined by each physician.
- Physician must confirm and/or edit each clinical concept to avoid the "default error".

Physicians' attitude towards innovative EMRs

- physicians, especially physicians who have a say on what system they can choose, do prefer EMRs with innovative approaches to data collection.
- Practices with more physicians tend to be more conservative.
Ⅱ· Data Visualization
How to present data to physicians to support “their mental model”?
EMRs don’t really distinguish fairly obvious differences


the IOM’s seven information-intensive aspects
- Stores comprehensive patient data
- provides cognitive support
- intergration of patient-specific data
- integration of evidence-based guidelines
- practice-wide care management
- population-level care management
- recognizing the home as a new care setting



Key Concepts/Vocabulary
Readings
Videos
2015-09-30 初稿, 完成一半视频
2015-10-01 完成所有视频